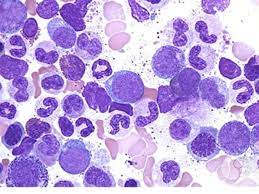
CHRONIC myeloid leukaemia (CML) is a cancer of the white blood cells that accounts for one in every eight leukaemia cases in Malaysia (Malaysian National Cancer Registry Report 2007-11).
Unlike most cancers, CML is a lifelong disease that can take a significant toll on patients — from their deteriorating health until the point of diagnosis, commencing treatment, treatment adherence and regular monitoring for disease response.
Advances in medicine have improved the treatment outcome of CML patients. CML patients are now treated with tyrosine kinase inhibitors (TKIs), a group of oral medicines that bind to the specific cancer protein, thus causing less damage to normal cells.
TKIs broke new ground in cancer treatment when they were discovered 20 years ago. Notably, the overall survival and quality of life of CML patients have improved. It is anticipated that CML patients can have a life span that is close to that of the normal population. Currently, the ideal goal of CML treatment is to have prolonged disease remission even after treatment discontinuation.
However, not all patients respond optimally to TKIs and some patients can also lose control of the disease after some time.
Not all CML patients achieve and maintain good response to treatment

Up to 50% of CML patients may need therapy changes during their disease’s clinical course. The five-year failure rate for first-line TKIs can be 30-50%, while the second and third-line TKIs have 60% and 70% five-year failure rates, respectively.
A suboptimal response is detected when a patient commences the first line of treatment but does not show optimal improvement within the first two years, or when the patient loses good control of the disease after being on the treatment for some time, thereby needing a change to the second or third line of TKI treatment.
This failure to respond to TKIs can be caused by resistance to the treatment or intolerance to the side effects of the TKI. In patients who required a switch to a third-line TKI, half of them were due to intolerance and the other half to TKI resistance.
Resistance to treatment happens when the genes of the cancer cells mutate, making the TKI unable to bind effectively to the cancer protein receptor site, much like how an arrow has lost its target.
Other factors that may complicate CML treatment and the choice of TKIs are patients’ existing comorbidities (such as heart diseases) that could limit the options for TKI therapy. To add to the treatment conundrum, the current conventional TKIs target the same receptor site on the cancer protein, and this may cause resistance to this class of drugs. When this happens, up to 30% of patients who initially respond to treatment end up becoming resistant.
The unmet needs
It has been 20 years since conventional TKIs made a significant impact on the lives of CML patients. However, there are still unmet needs for those CML patients undergoing later-line treatments with the current available options.
What we are hoping to achieve, especially with later-line treatments, is better disease control, lower failure rates and fewer side effects.
What we have learned with CML is that the quicker we bring the disease under control, the better the chance of success in attaining higher remission rates, overall survivability, and a better quality of life for our patients.
To help our patients navigate their journey successfully, we need to develop more options for CML patients. — May 24, 2023
Datuk Dr Chang Kian Meng is a consultant haematologist at Sunway Medical Centre.
The views expressed are solely of the author and do not necessarily reflect those of Focus Malaysia.