THE Health Ministry (MOH) and World Health Organisation (WHO) recently co-published a report titled, The Direct Health-Care Cost of Non-Communicable Diseases (NCD) in Malaysia.
The report, using data from 2019, shows what could well be deemed as a “depressing” amount of Government spending on only three NCDs categories (estimated to be at RM9.65 bil).
The data shows that the three selected NCDs and related Government spending were as follows:
- Diabetes – which incurred the highest cost at RM4.38 bil (45.38% of the total)
- Cardiovascular disease (CVD) – at RM3.93 bil (40.73%)
- Cancer – at RM1.34 bil (13.8%).
The findings are already worrying even without the inclusion of other NCDs deemed relatively not as common, such as chronic respiratory diseases, mental health and osteoarthritis, which were not included in the RM9.65 bil figure.
The MOH has estimated that for 2017, these three NCDs cost Malaysia up to RM12.88 bil in productivity losses due to absenteeism, presenteeism and premature deaths. This makes the combined cost of the three NCD categories in 2017 to be RM22.53 bil to the Malaysian economy.
We must look at the NCDs’ risk factors to understand why this is happening.
“Burden of disease”
According to the WHO, the risk of dying from an NCD can increase due to tobacco use, lack of physical activity, excessive use of alcohol and unhealthy diets. Moreover, 77% of all NCD fatalities come from low- and middle-income countries.

Similarly, a 2020 MOH report also revealed that the “burden of disease” (i.e. highly possible causes) of the three selected NCDs has the same four attributable risk factors.
For CVD, unhealthy diets accounted for 62.1% of the burden of disease, whereas tobacco use accounted for 24.8%. The same goes for diabetes – unhealthy diets and tobacco use accounted for the most burden of disease at 39.7% and 18.5%, respectively.
As for cancer, tobacco consumption accounted for the highest burden of disease at 18%, while unhealthy diets accounted for 8.33%.
However, because the combined effects of the risk factors have not been considered, the related percentages are not to be regarded as cumulative.
Low physical activity was not a prominent risk factor while alcohol use was only a relatively minor contributor among the three NCD categories.
Unhealthy diets, the most prominent risk factor for CVD and diabetes, could be caused by the high cost of eating healthy food which makes it unaffordable for the low-income group.
According to a 2019 survey done by Food Industry Asia (FIA) and research firm IGD, despite 99% of Malaysian respondents indicating interest in trying to improve their eating habits, 71% identified cost as a key barrier.
“Not eating enough veges”
Moreover, according to the National Health and Morbidity Survey (NHMS) 2019, 95% of Malaysians do not consume enough vegetables, as recommended by the MOH. Most only eat one type of vegetable and do not eat fruit and vegetables according to the recommended portions servings (quarter grains, quarter protein and half fruits and vegetables).

According to Deputy Health Minister Datuk Dr Noor Azmi Ghazali, eating only one type of vegetable per meal is not sufficient as it can result in “under-nutrition” and excessive consumption of sugar and simple carbohydrates causes organic compounds to be stored as fat in the body, leading to NCDs, especially the three major ones (diabetes, CVD and cancer).
Moreover, Malaysia is known to be the “fattest” nation in ASEAN, with one in two Malaysian adults being overweight or obese. In addition, according to the NHMS 2019, children from bottom 40 income (B40) households had obesity and overweight prevalence rates of 15.6% and 15.4%, respectively.
Universiti Kebangsaan Malaysia (UKM)’s Nutritional Science programme professor of nutrition Dr Ruzita Abd Talib said in addition to increasing the risk of obesity in children, poor eating choices could also increase their risk of developing diabetes and other NCDs.
She further stated that obesity could also be induced by food insecurity (due to finances which then influence the dietary choices) when lower-income groups choose to eat energy-dense food with high fat and sugar contents since these are easier to obtain, cheaper and satiate hunger quicker.
Furthermore, according to the 2021 Health Literacy in Malaysia: A Population-Based Study, based on a cross-sectional population-based survey conducted as part of the NHMS 2019, 37.7% of the B40 group had limited health illiteracy – the highest among the income groups.
Besides that, limited health literacy was more prominent among respondents in the older age group and lower education levels.
Additionally, individuals with lower levels of education and older age groups were also more likely to have limited health literacy.
“Addressing the root of the problem”
To reduce the impact of NCDs on our economy, the MOH has sought to address the problem from the root cause. One of the critical ways is to improve Malaysians’ dietary habits and lifestyles.
The MOH has introduced the Healthier Choices Logo (HCL) in April 2017. It is a criteria-based front-of-pack scheme that aims to give point-of-sales information so that it is easier for consumers to make an informed decision. But we can do more.
It should introduce front-of-pack warning labels. The labels provide information on the specific compositions and structures of the foods concerned – for example, whether these are high or low in saturated fat, salt and sugar.
Several countries have implemented or plan to implement front-of-package warning labels on unhealthy food to lessen the unsustainable burden that bad diets place on society. This measure builds on the front-of-package nutrition labelling already in use in the UK:
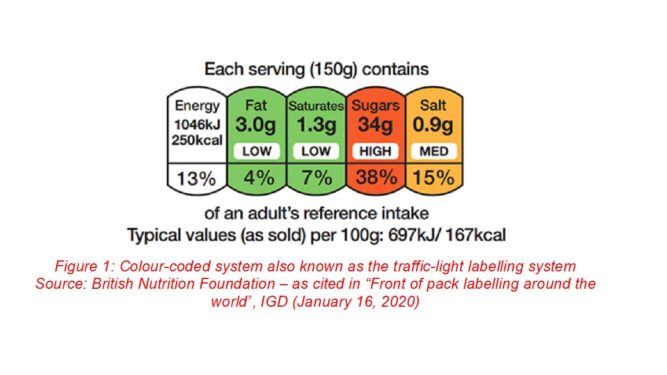
In addition, the front of package labelling should incorporate an “ultra-processed” warning label such as, “Warning: this product is ultra-processed and it is high in (saturated fat/salt/sugar)”, as recommended by BMJ Global Health:

The additional label or extra wording would “signal an independent, additional measure of unhealthiness”. Such labelling also further serves to enhance the health literacy of consumers based on the level of food processing.
However, as highlighted before, the affordability of unhealthy food makes it a readily and easily accessible alternative and source of diet for the B40 group, the lowest income group with limited health illiteracy.
Therefore, instead of only promoting healthier dietary choices and habits, the MOH should go a step further as part of what should be a full-spectrum policy effort by a lateral focus on introducing front-of-package warning labels with respect to unhealthy and ultra-processed foods.
Since unhealthy diets can be said to be the primary risk factor for the major NCDs, it is vital that we seriously tackle the root cause of the problem by adopting a strategy that is similar to combating smoking (which is also a major cause, including Type 2 Diabetes, no less).
Labelling which informs and warns is equally necessary if we want to carry the war beyond healthcare and towards preventative measures. After all, “prevention is better than cure”. – Aug 28, 2022
Jason Loh and Anis Salwana Abdul Malik are part of the research team of EMIR Research, an independent think tank focused on strategic policy recommendations based on rigorous research.
The views expressed are solely of the author and do not necessarily reflect those of Focus Malaysia.
Main photo credit: Healthline










